What is Sepsis?

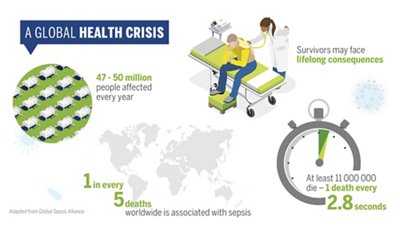
Sepsis is the body’s extreme response to an infection. It is a life-threatening organ dysfunction caused by a dysregulated host response to an infection. Though many people may not be aware of it, sepsis is one of the primary causes of death throughout the world, it is estimated that one in every five deaths worldwide is associated with sepsis.1
Sepsis is a global burden and a major health problem because of its high mortality, morbidity, and high incidence. It affects around 49 million people each year, leading to more than 11 million deaths.2 Sepsis can lead to severe sepsis and septic shock. Approximately 30% of patients diagnosed with severe sepsis do not survive, 3 and up to 50% of survivors suffer from post-sepsis syndrome. It progresses rapidly, and life-saving efforts can have negative impacts on long-term challenges like antimicrobial resistance. In 2017, the World Health Organization (WHO) declared sepsis as a Global Health Priority.4
Learn More about sepsis for healthcare professionals in our Medical Education section.
How does Sepsis occur?
Sepsis can be caused by bacteria, virus, or fungi. There are four types of infections that are most often linked to sepsis: lung infections such as pneumonia, skin infections, gut infections, and urinary tract infections (UTIs). Different types of bacteria can cause these infections, but the most common bacteria associated with sepsis are Escherichia coli, Staphylococcus, and Streptococcus. The most common underlying cause of sepsis-related death is lower respiratory infections causing pneumonia.5
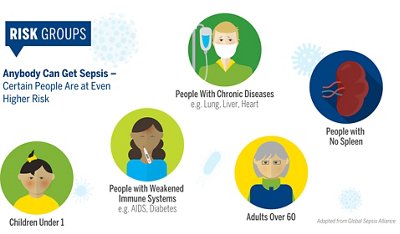
Anyone can get an infection, and almost any infection can lead to sepsis. However, there are some groups of risk who may be more likely to get sepsis, mainly because they are at a higher risk.
The six typical sepsis indicators include:
- Slurred speech or confusion
- Extreme shivering or muscle pain, fever
- Passing no urine all day
- Severe breathlessness
- Extreme pain and discomfort
- Skin mottled or discolored
Since these symptoms are non-specific and can be confused with other conditions, sepsis is often difficult to recognize and diagnose at early stages, when it is still potentially reversible.7
What is the healthcare burden of Sepsis?
As a leading cause of morbidity and mortality with millions of cases a year, sepsis has a substantial economic impact on healthcare systems due to prolonged hospital stays and intensive treatments.
For example, in the United States:
- Sepsis is the #1 cost of hospitalization with an estimated $62 billion annually spent on acute sepsis hospitalization and skilled nursing care.7
- There is a substantial amount of additional costs after discharge for many patients.7
- The average cost per hospital stay for sepsis is double the average cost per stay for all other conditions.7
- Sepsis is the primary cause of readmission to the hospital, costing more than $3.5 billion each year.7
Why should you care about Sepsis?
As is the case in any medical emergency, accurate diagnosis and prompt treatment are critical to ensure the best possible outcomes for patients. Until a cure for sepsis is found, early detection and treatment are essential for survival and to limiting disability caused by sepsis to survivors.7
Initiating and adapting therapy in a timely manner reduces mortality and lowers incidence and severity of long-term symptoms (post-sepsis syndrome).8 It potentially limits unnecessary tests and treatments, shortens hospital stays, and supports antimicrobial stewardship.
In a race against the clock, culture-based diagnosis is not fast enough, and so, in recent years, major efforts have been made to find solutions that allow rapid and accurate diagnosis of this disease. Timely diagnosis is required to adjust treatment, and the delayed results of traditional bacterial cultures and AST remain one of the major barriers to the prompt initiation of appropriate therapy.
Early detection and treatment are absolutely essential to improve both the human and economic impact of sepsis.
Why should you consider Sepsis Solutions from bioMérieux?
Our innovations have positively disrupted conventional sepsis management diagnostics processes providing a much more rapid blood culture, pathogen identification (ID), and antimicrobial susceptibility testing (AST). Rapid diagnostics enables early therapy decision for optimal septic patient management, to support your institution and hospitalization cost savings, preserve the effectiveness of antibiotics, and prevent antimicrobial resistance.
bioMérieux provides the most comprehensive sepsis diagnostics solution in the market offering faster, actionable decision-making information and diagnostics to leverage optimized therapy and patient care for sepsis patients.
We are the partner you can count on for sepsis management. Our solution brings:
- Early therapy decision for optimal septic patient management: Clinicians need diagnostic insights rapidly for timely, appropriate therapy for sepsis. Streamline workflow with the latest diagnostic solutions for rapid identification (ID) and antimicrobial susceptibility testing (AST) directly from positive blood cultures.
- Full integration for increased workflow efficiency and potential hospitalization cost savings: Informed clinical decisions mean improved patient outcomes, with reduced length of therapy and hospital stays. Impact sepsis patient management with rapid and reliable ID & AST solutions that fit your lab workflow and are part of an integrated sepsis solution.
Our Sepsis Solution
Optimize antibiotic therapy for better patient care and enhanced sepsis management in your institution with the bioMérieux Sepsis Solution.
Complete Sepsis Solution by Patient Pathway

SEPSIS Solution
METROMAPS SEPSIS 01
Disclaimer: Product availability varies by country. Please consult your local bioMérieux representative for product availability in your country.
The first step in the management of sepsis is to collect the samples and administer empiric therapy. Within the first hour of recognition of sepsis, in most cases the causative agent is unknown, and broad-spectrum antibiotic therapy is indicated. In conjunction with initial clinical assessments, bioMérieux provides the diagnostic tools to aid in the accuracy of early diagnosis and enable more appropriate clinical decisions for a targeted therapy sooner.
-
VIDAS® B•R•A•H•M•S PCT™
Important Biomarker for Improved Patient Management
Detects procalcitonin, a biomarker that aids in the risk assessment for progression to severe sepsis and septic shock. PCT also aids in decision making on antibiotic therapy for patients with lower respiratory tract infections (LRTI).
-
BIOFIRE® FILMARRAY® Meningitis/Encephalitis Panel
1 Test. 14 Targets. ~1 Hour.
The BIOFIRE ME Panel provides answers on 14 of the most common bacterial, viral, and yeast pathogens that cause central nervous system infections to help healthcare providers rapidly distinguish between bacterial and viral meningitis and optimize life-saving therapy.
-
BIOFIRE® FILMARRAY® Pneumonia & Pneumonia plus Panels
1 Test. Up to 34 Targets. ~1 Hour.
Syndromic tests targeting a comprehensive menu of bacteria and viruses that cause pneumonia and other lower respiratory tract infections, as well as 7 genetic markers of antibiotic resistance.
-
BIOFIRE® Respiratory 2.1 and 2.1plus Panels
1 Test. Up to 23 Targets. ~45 Minutes.
The BIOFIRE RP2.1 and RP2.1plus Panels use the syndromic approach to accurately detect and identify the pathogens most associated with respiratory infections. Fast and comprehensive results may enable better-informed diagnosis and treatment of patients.
After initial risk assessment and administration of empiric therapy, pathogen detection, identification, and susceptibility testing provide critical information about whether the initial therapy needs to be adjusted. This is especially important because a patient may have an infection that is resistant to certain antibiotics, and because it allows physicians to optimize therapy sooner.
-
BACT/ALERT® 3D
Accurate Blood Culture Results
BACT/ALERT® 3D brings flexible and modular automated detection systems for any size laboratory that needs to meet blood culture guidelines efficiently, economically, and effectively.
-
BACT/ALERT® VIRTUO®
Automated System for Faster Blood Culture
The first fully automated blood culture system, helping to refine and redesign laboratory workflow to maximize efficiency, while providing the fastest clinically impactful results on the market.1,2
-
MAESTRIA™
New Generation Microbiology Middleware
An innovative, integrated software solution designed to orchestrate your lab routine and transform data into insights.
-
PREVI® COLOR GRAM
A Market-Leading Automated Gram Stainer Offering Confidence in Results
Gram staining is a key step in your microbiology workflow, and PREVI® COLOR GRAM is the system to streamline it and provide timely staining results for impactful decisions.
-
BIOFIRE® Blood Culture Identification 2 Panel
1 Test. 43 Targets. ~1 Hour.
The BIOFIRE BCID2 Panel tests for 43 targets associated with bloodstream infections, including Gram-negative bacteria, Gram-positive bacteria, yeast, and 10 antimicrobial resistance genes – all with one test and with results available in about an hour from positive blood culture.
-
VITEK® MS PRIME
New-Generation Mass Spectrometry Microbial Identification System
VITEK® MS PRIME combines microbiology expertise with innovation taking mass spectrometry to the next level by maximizing the impact of daily laboratory workflow for better patient care.
-
VITEK® 2
Fully integrated Identification and Antimicrobial Susceptibility Testing
VITEK® 2, the leading automated system for routine antimicrobial susceptibility testing, provides efficient workflow, faster AST results. Its fully-integrated ID & AST approach ensures superior performance to rapidly and confidently guide therapy.
-
VITEK® REVEAL™
Rapid Antimicrobial Susceptibility Testing (AST) for Bloodstream Infections
The newest addition to our Sepsis Solution, VITEK® REVEAL™ offers rapid AST results to effectively and efficiently manage bloodstream infections.
-
VIDAS® B•R•A•H•M•S PCT™
Important Biomarker for Improved Patient Management
Detects procalcitonin, a biomarker that aids in the risk assessment for progression to severe sepsis and septic shock. PCT also aids in decision making on antibiotic therapy for patients with lower respiratory tract infections (LRTI).
In the case of sepsis, it is critically important that clinicians assess when to discontinue antibiotics. VIDAS® B•R•A•H•M•S PCT has been cleared by the FDA to aid in decision making on antibiotic discontinuation for patients with suspected or confirmed sepsis.
-
VIDAS® B•R•A•H•M•S PCT™
Important Biomarker for Improved Patient Management
Detects procalcitonin, a biomarker that aids in the risk assessment for progression to severe sepsis and septic shock. PCT also aids in decision making on antibiotic therapy for patients with lower respiratory tract infections (LRTI).
-
VILINK®
Optimize Instrument UPTIME to Improve Laboratory Productivity
A secure solution offering remote access, proactive maintenance, and remote updates. VILINK® diagnoses, solves software and instrument issues, and supports your systems to enable laboratory productivity and efficiency improvements.
-
BIOMÉRIEUX LAB CONSULTANCY
Microbiology Expertise and Consultancy to Optimize Lab Performance
Transforming laboratories together to control costs, maximize quality, shorten time to result, and empower staff.
Integrated Offer
Our comprehensive diagnostics solution is backed up by advanced analytics, services, and educational modules to help hospital and laboratories overcome their challenges, reinforced by our promise to be a committed service partner for all our products from consultancy to installation, connectivity, training, verification, and customer service, to help you on optimized time to therapy for better patient care.
bioMérieux
Sepsis Solutions
Useful Resources on Sepsis Solutions
Contact Us About Our Sepsis Solutions
Contact Us
References
1. Zick, Marvin. “The Lancet: Sepsis Associated with 1 in 5 Deaths Worldwide, Double Prior Estimates – Children and Poor Regions Hit Hardest.” Global Sepsis Alliance. Global Sepsis Alliance, January 16, 2020.
2. Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet (London, England). 2020;395(10219):200-11.z
3. Vincent JL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–353.
4. World Health Organization. WHO Report on the burden of endemic health care-associated infection worldwide. 2017-11-21 15:11:22 2011.
5. Turk J Med Sci. 2021; 51(7): 3301–3311. Published online 2021 Dec 17. doi: 10.3906/sag-2108-239
6. Sepsis Alliance. Sepsis and Long-Term Care. 2022. https://www.sepsis.org/sepsisand/sepsis-long-term-care/
7. Sepsis Alliance. What is Sepsis. 2022. https://www.sepsis.org/sepsis-basics/what-is-sepsis/
8. Evans L, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. PubMed Central, 2021.